Dynamic CFD model of reactor membrane and corresponding WSS. Source [3]
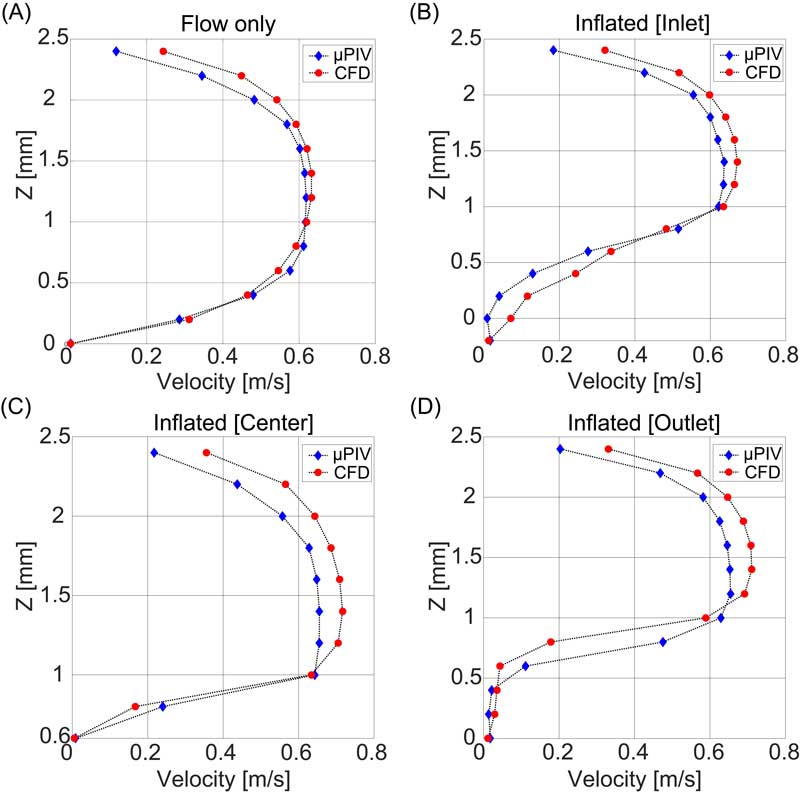
Figure 1. Validation of the velocity field. Comparison of Computational Fluid Dynamics simulation (CFD) and μPIV flow profiles at 0.4 l/min flow. (A) CFD (red circles) and μPIV (blue rhombus) profiles for the flat membrane configuration. (B-D) Corresponding profiles for the configuration with membrane inflated to 20% extension (i.e. 720 mbar) at the inlet (B), center (C) and outlet (D) respectively. Source [3]
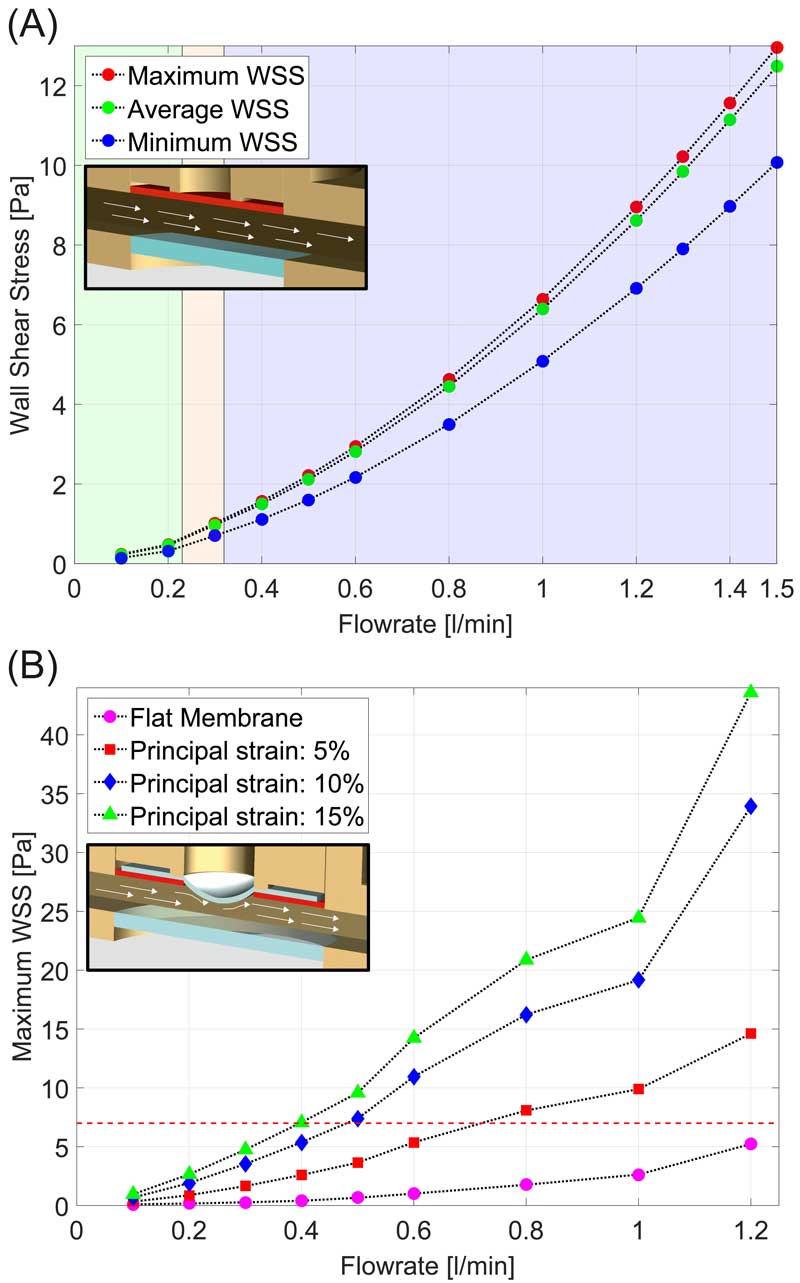
Figure 2. WSS profiles in the reactor. (A) Maximum (red circles), average (green circles) and minimum (blue circles) WSS at the surface of the deformable membrane as a function of pure flow rate (flow rates from 0.1 l/min to 1.5 l/min) in the flat membrane configuration. (B) Maximum WSS at the surface of the deformable membrane as function of the flow rate and for different membrane strain conditions ranging from flat (pink circles) up to surface strain of 15% (green triangles). Source [3]
Christian Loosli
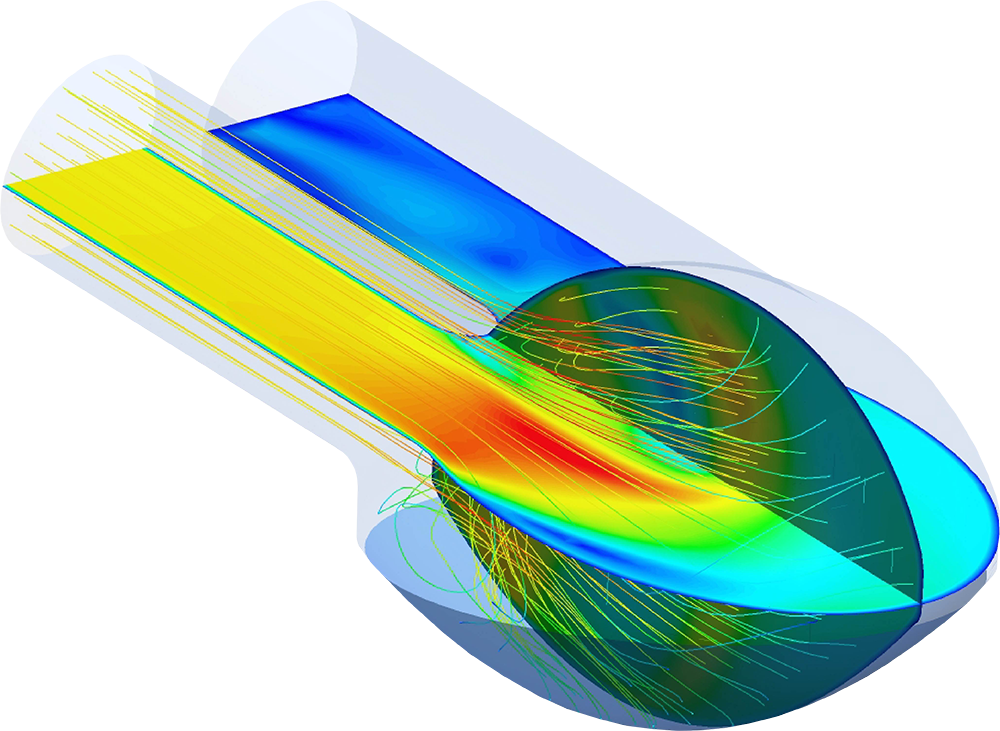
Flow field within a pulsatile ventricular assisted device.
Description:
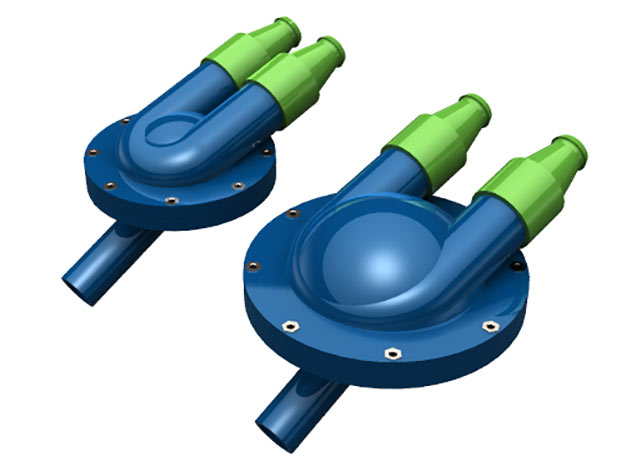
The objective of this task is to design, fabricate and validate a blood propulsion device based on pulsatile hybrid membrane. Several studies for pulsatile ventricular assist devices are already performed focusing on residence time, chamber shape to minimize the thrombotic risk, washout efficiency. The challenge in our project lies in designing and realizing a viable concept that minimizes the in-plane deformation and wall shear stress (WSS) in the hyperelastic hybrid membrane. Dynamic CFD and finite element models of the pump and the blood are created and employed to first analyze and then minimize these parameters by adapting the pump geometry based on representative boundary conditions and actuation strategies. Thereby, a fluid structure interaction (FSI) model will be established. We compare our flow simulation results with flow field measurements which we perform in the phase contrast magnet resonance imaging (PC-MRI). For the characterization of the membrane deformation, we use the Digital Image Correlation techniques (DIC).
Christian Loosli
Description:
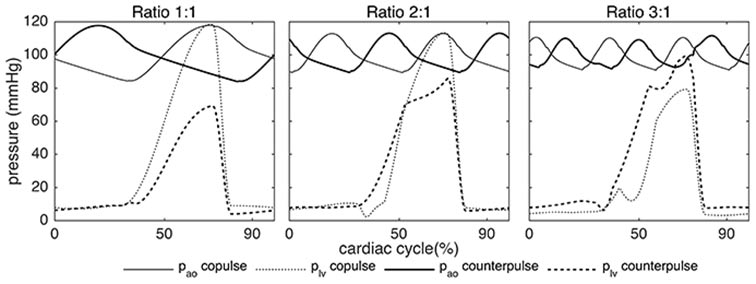
Besides concerns of thrombus formation inside the pump cavity and mechanical longevity, the main drawback of pVADs is their physical size and weight which preclude or greatly compromise their implantation for the majority of patients. The resulting paracorporeal usage presents a high risk of infection as well as a physical and psychological burden for the recipients. The size of the pVAD is closely linked to the required stroke volume, which in turn is determined by the demanded pump flow and stroke rate. We propose a reduction of the stroke volume to increase the feasibility of full pVAD implantation while maintaining the pVAD's support capability by increasing the pump's stroke rate. Simulations show that the volume of a simulated synchronized pVAD can be reduced to 29% of its original volume by using a higher pump frequency that is 3-times the physiological heart rate and preferable actuation settings. Source [1]
Mathias Rebholz
Publication:
A Novel Interface for Hybrid Mock Circulations to Evaluate Ventricular Assist Devices.
Gregor Ochsner, Raffael Amacher, Alois Amstutz, Andre Plass, Marianne Schmid Daners, Hendrik Tevaearai, Stijn Vandenberghe, Markus J. Wilhelm, and Lino Guzzella
IEEE transactions on biomedical engineering, 60.2 (2013): 507-516.
DOI
A Robust Reference Signal Generator for Synchronized Ventricular Assist Devices.
Raffael Amacher, Gregor Ochsner, Antonio Ferreira, Stijn Vandenberghe, and Marianne Schmid Daners
IEEE Transactions on Biomedical Engineering, 60.8 (2013): 2174-2183.
DOI
Control of ventricular unloading using an electrocardiogram-synchronized Thoratec paracorporeal ventricular assist device
Raffael Amacher, Alberto Weber, Henriette Brinks, Shannon Axiak, Antonio Ferreira, Lino Guzzella, Thierry Carrel, James Antaki, Stijn Vandenberghe
The Journal of Thoracic and Cardiovascular Surgery, 146.3 (2013): 710 – 717
DOI